Clinically, meningitis manifests with
meningeal symptoms (eg, headache, nuchal rigidity, photophobia), as
well as pleocytosis (an increased number of white blood cells) in the
cerebrospinal fluid (CSF). Depending on the duration of symptoms,
meningitis may be classified as acute or chronic. (See Etiology and
Clinical Presentation.)
For empiric antifungal therapy, the Centers for Disease Control (CDC) recommends voriconazole, preferably at a dose of 6 mg/kg every 12 hours, continued for the duration of treatment. Serum voriconazole concentrations should be monitored regularly (eg, weekly), with a target trough level of 2-5 mcg/ml.[4]
For additional information on the treatment of fungal meningitis, see the discussion of Exserohilum rostratum in Meningitis Treatment.
Continuing updates on fungal infection published by the CDC can be obtained at the CDC Web page Multisite Fungal Meningitis Outbreak Investigation.
See the images of meningitis below.
 Pneumococcal meningitis in a patient with alcoholism. Courtesy of the CDC/Dr. Edwin P. Ewing, Jr.
Pneumococcal meningitis in a patient with alcoholism. Courtesy of the CDC/Dr. Edwin P. Ewing, Jr. 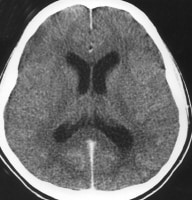 Acute bacterial meningitis. This axial nonenhanced computed tomography scan shows mild ventriculomegaly and sulcal effacement
Acute bacterial meningitis. This axial nonenhanced computed tomography scan shows mild ventriculomegaly and sulcal effacement 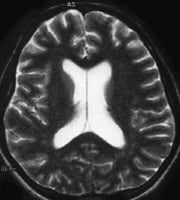 Acute bacterial meningitis. This axial T2-weighted magnetic resonance image shows only mild ventriculomegaly.
Acute bacterial meningitis. This axial T2-weighted magnetic resonance image shows only mild ventriculomegaly. 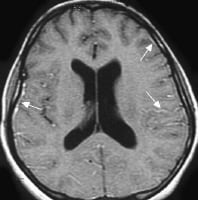 Acute
bacterial meningitis. This contrast-enhanced, axial T1-weighted
magnetic resonance image shows leptomeningeal enhancement (arrows). Meningitis
is a clinical syndrome characterized by inflammation of the meninges, 3
layers of membranes that enclose the brain and spinal cord. They
consist of the following:
Acute
bacterial meningitis. This contrast-enhanced, axial T1-weighted
magnetic resonance image shows leptomeningeal enhancement (arrows). Meningitis
is a clinical syndrome characterized by inflammation of the meninges, 3
layers of membranes that enclose the brain and spinal cord. They
consist of the following:
Meningitis can also be divided into the following 3 general categories:
Pyogenic (bacterial) meningitis consists of inflammation of the meninges and the underlying subarachnoid CSF. If not treated, bacterial meningitis may lead to lifelong debility or death.[5] [6] The disease was uniformly fatal before the antimicrobial era, but with the advent of antimicrobial therapy, the overall mortality rate from bacterial meningitis has decreased. Nonetheless, it remains alarmingly high, being approximately 25%. (See Epidemiology.)
The emergence of resistant bacterial strains has prompted changes in antibiotic protocols in some countries, including the United States. Apart from dexamethasone, neuronal cell protectants still hold only future promise as adjunctive therapy. (See Treatment and Management and Medication.)
The specific infective agents that are involved in bacterial meningitis vary among different patient age groups, and the inflammation may evolve into the following conditions (see the images below):
For more information, see the following:
Go to Viral Meningitis for complete information on this topic.
When the cause of aseptic meningitis is discovered, the disease can be reclassified according to its etiology. If appropriate diagnostic methods are performed, a specific viral etiology is identified in 55-70% of cases of aseptic meningitis. However, the condition can also be caused by bacterial, fungal, mycobacterial, and parasitic agents.
from http://emedicine.medscape.com
Fungal meningitis update
Although iatrogenic meningitis has typically been a complication of neurosurgical procedures, an outbreak of fungal meningitis has resulted from epidural injection of a contaminated methylprednisolone solution. The outbreak, which has, at this point, involved 308 cases and 23 deaths in 17 states, originated with preparations from a single compounding pharmacy.[1, 2] Pathogens in these cases have been identified as Exserohilum rostratum (a brown-black mold) and Aspergillus.[3]For empiric antifungal therapy, the Centers for Disease Control (CDC) recommends voriconazole, preferably at a dose of 6 mg/kg every 12 hours, continued for the duration of treatment. Serum voriconazole concentrations should be monitored regularly (eg, weekly), with a target trough level of 2-5 mcg/ml.[4]
For additional information on the treatment of fungal meningitis, see the discussion of Exserohilum rostratum in Meningitis Treatment.
Continuing updates on fungal infection published by the CDC can be obtained at the CDC Web page Multisite Fungal Meningitis Outbreak Investigation.
Meningitis overview
Infections of the central nervous system (CNS) can be divided into 2 broad categories: those primarily involving the meninges (meningitis) and those primarily confined to the parenchyma (encephalitis).See the images of meningitis below.
 Pneumococcal meningitis in a patient with alcoholism. Courtesy of the CDC/Dr. Edwin P. Ewing, Jr.
Pneumococcal meningitis in a patient with alcoholism. Courtesy of the CDC/Dr. Edwin P. Ewing, Jr. 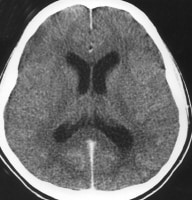 Acute bacterial meningitis. This axial nonenhanced computed tomography scan shows mild ventriculomegaly and sulcal effacement
Acute bacterial meningitis. This axial nonenhanced computed tomography scan shows mild ventriculomegaly and sulcal effacement 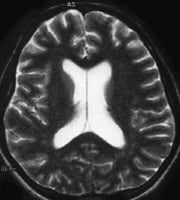 Acute bacterial meningitis. This axial T2-weighted magnetic resonance image shows only mild ventriculomegaly.
Acute bacterial meningitis. This axial T2-weighted magnetic resonance image shows only mild ventriculomegaly. 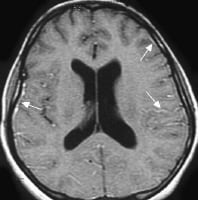 Acute
bacterial meningitis. This contrast-enhanced, axial T1-weighted
magnetic resonance image shows leptomeningeal enhancement (arrows). Meningitis
is a clinical syndrome characterized by inflammation of the meninges, 3
layers of membranes that enclose the brain and spinal cord. They
consist of the following:
Acute
bacterial meningitis. This contrast-enhanced, axial T1-weighted
magnetic resonance image shows leptomeningeal enhancement (arrows). Meningitis
is a clinical syndrome characterized by inflammation of the meninges, 3
layers of membranes that enclose the brain and spinal cord. They
consist of the following: - Dura - A tough outer membrane
- Arachnoid - A lacy, weblike middle membrane
- Subarachnoid space - A delicate, fibrous inner layer that contains many of the blood vessels that feed the brain and spinal cord
- Age of 60 years or greater
- Age of 5 years or less
- Diabetes mellitus, renal or adrenal insufficiency, hypoparathyroidism, or cystic fibrosis
- Immunosuppression, which increases the risk of opportunistic infections and acute bacterial meningitis
- Human immunodeficiency virus (HIV) infection, which predisposes to bacterial meningitis caused by encapsulated organisms, primarily S pneumoniae, and opportunistic pathogens
- Crowding (eg, military recruits and college dorm residents), which increases the risk of outbreaks of meningococcal meningitis
- Splenectomy and sickle cell disease, which increase the risk of meningitis secondary to encapsulated organisms
- Alcoholism and cirrhosis
- Recent exposure to others with meningitis, with or without prophylaxis
- Contiguous infection (eg, sinusitis)
- Dural defect (eg, traumatic, surgical, congenital)
- Thalassemia major
- Intravenous (IV) drug abuse
- Bacterial endocarditis
- Ventriculoperitoneal shunt
- Malignancy (increased risk of Listeria species infection)
- Some cranial congenital deformities
Meningitis can also be divided into the following 3 general categories:
- Pyogenic (bacterial)
- Granulomatous
- Lymphocytic
Pyogenic (bacterial) meningitis consists of inflammation of the meninges and the underlying subarachnoid CSF. If not treated, bacterial meningitis may lead to lifelong debility or death.[5] [6] The disease was uniformly fatal before the antimicrobial era, but with the advent of antimicrobial therapy, the overall mortality rate from bacterial meningitis has decreased. Nonetheless, it remains alarmingly high, being approximately 25%. (See Epidemiology.)
The emergence of resistant bacterial strains has prompted changes in antibiotic protocols in some countries, including the United States. Apart from dexamethasone, neuronal cell protectants still hold only future promise as adjunctive therapy. (See Treatment and Management and Medication.)
The specific infective agents that are involved in bacterial meningitis vary among different patient age groups, and the inflammation may evolve into the following conditions (see the images below):
- Ventriculitis
- Empyema
- Cerebritis
- Abscess formation
 Chronic
mastoiditis and epidural empyema in a patient with bacterial
meningitis. This axial computed tomography scan shows sclerosis of the
temporal bone (chronic mastoiditis), an adjacent epidural empyema with
marked dural enhancement (arrow), and the absence of left mastoid air.
Chronic
mastoiditis and epidural empyema in a patient with bacterial
meningitis. This axial computed tomography scan shows sclerosis of the
temporal bone (chronic mastoiditis), an adjacent epidural empyema with
marked dural enhancement (arrow), and the absence of left mastoid air. 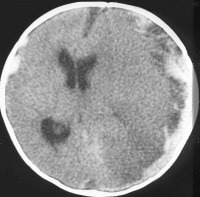 Subdural
empyema and arterial infarct in a patient with bacterial meningitis.
This contrast-enhanced axial computed tomography scan shows left-sided
parenchymal hypoattenuation in the middle cerebral artery territory,
with marked herniation and a prominent subdural empyema.
Subdural
empyema and arterial infarct in a patient with bacterial meningitis.
This contrast-enhanced axial computed tomography scan shows left-sided
parenchymal hypoattenuation in the middle cerebral artery territory,
with marked herniation and a prominent subdural empyema.
Acute bacterial meningitis
Acute bacterial meningitis denotes a bacterial cause of this syndrome. This is usually characterized by an acute onset of meningeal symptoms and neutrophilic pleocytosis. Depending on the specific bacterial cause, the syndrome may be called, for example, any of the following:- Pneumococcal meningitis
- Haemophilus influenzae meningitis
- Staphylococcal meningitis
- Meningococcal meningitis
- Tuberculous meningitis
For more information, see the following:
- Meningococcal Meningitis
- Staphylococcal Meningitis
- Haemophilus Meningitis
- Tuberculous Meningitis
Subacute bacterial meningitis
Most bacterial meningitis is not acute. Approximately 75% of patients with bacterial meningitis present subacutely, with symptoms beginning several days prior. These ill patients still require urgent ED diagnosis and care to prevent further decompensation.Meningitis caused by nonbacterial organisms
Fungal and parasitic causes of meningitis are also termed according to their specific etiologic agent, such as cryptococcal meningitis, Histoplasma meningitis, and amebic meningoencephalitis.Viral meningitis
If, after an extensive workup, aseptic meningitis is found to have a viral etiology, it can be reclassified as a form of acute viral meningitis (eg, enterovirus meningitis, herpes simplex virus [HSV] meningitis).Go to Viral Meningitis for complete information on this topic.
Aseptic meningitis
In many cases, a cause for meningitis is not apparent after initial evaluation and is therefore classified as aseptic meningitis. These patients characteristically have an acute onset of meningeal symptoms, fever, and cerebrospinal pleocytosis that is usually prominently lymphocytic.When the cause of aseptic meningitis is discovered, the disease can be reclassified according to its etiology. If appropriate diagnostic methods are performed, a specific viral etiology is identified in 55-70% of cases of aseptic meningitis. However, the condition can also be caused by bacterial, fungal, mycobacterial, and parasitic agents.
Chronic meningitis
Chronic meningitis is a constellation of signs and symptoms of meningeal irritation associated with CSF pleocytosis that persists for longer than 4 weeks.from http://emedicine.medscape.com


0 comments
Post a Comment